Pain Management: Everything You Ever Needed to Know Before Treatment
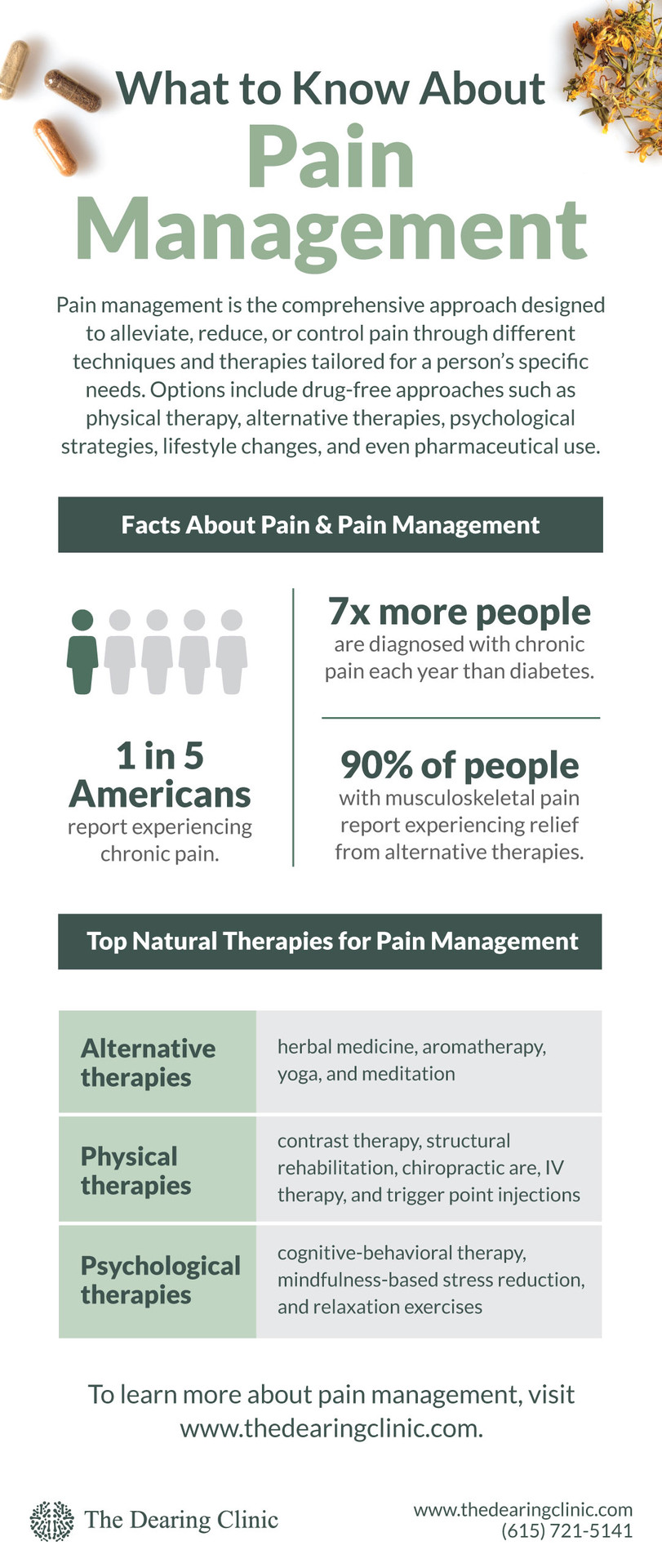
Pain management is the comprehensive approach designed to alleviate, reduce, or control pain through different techniques and therapies tailored for a person’s specific needs. Options include drug-free approaches such as physical therapy, alternative therapies, psychological strategies, lifestyle changes, and even pharmaceutical use.


Pain management is the comprehensive approach designed to alleviate, reduce, or control pain through different techniques and therapies tailored for a person’s specific needs. Options include drug-free approaches such as physical therapy, alternative therapies, psychological strategies, lifestyle changes, and even pharmaceutical use.
Whether it’s a headache, a muscle strain, or chronic lower back pain, whenever you experience any type of pain, it takes both a physical and emotional toll, making it only natural to want immediate relief. But did you know that there are many different pain management options available to you?
That’s right, you aren’t limited to grabbing that bottle of ibuprofen or acetaminophen for more acute pain concerns, nor do you have to feel resigned to turning to pharmaceutical painkillers or even surgery for more serious, chronic pain issues. The truth of the matter is that, depending on the source of your pain, you may benefit from other options.
But in order to determine what pain management solution is best for your situation, you must first understand what’s causing your pain so that you can decide which solution will be most effective.
So, let’s take a closer look at what causes pain and types of pain management available to you. We’ll also review what pain management doctors do to help you find relief so you can make the most informed decision possible for your care.
The Physiology of Pain
Before we can dive into pain management strategies, let’s first understand how the body experiences pain.
Experiencing pain involves the nervous system, brain, and other bodily processes, and it serves as a warning signal, alerting you to any potential injury or harm to your body. Whenever you experience pain, it’s the result of a very involved process that begins with the activation of specialized nerve endings called nociceptors, which are found throughout your body. When these nociceptors detect potential harm to your body (e.g., extreme temperatures or pressure), they send electrical signals to your spinal cord and brain.
Once these signals reach your spinal cord, they are transmitted to your brain, which then processes these signals and interprets them as pain. Interestingly, your brain is able to control your perception of pain, meaning it can increase or decrease the intensity of the pain you experience. And this ability to control your perception is influenced by different factors, including your emotions, thoughts, and past experiences.
What Causes Pain
Now that you know how you experience pain, let’s take a closer look at what causes pain.
Did you know that 1 in 5 Americans report experiencing chronic pain? In fact, research has shown that seven times more people are diagnosed with chronic pain each year than diabetes!
But all pain doesn’t happen the same way.
Pain can be triggered by numerous factors, including injuries, illnesses, inflammation, and even stress. Identifying the cause of your pain is the first step towards achieving pain relief.
When it comes to injuries, pain is your body’s way of protecting itself by alerting you to potential harm. For example, if you accidentally touch a hot stove, the pain you feel is your body’s way of telling you to move your hand to prevent further damage. In this case, pain serves as a warning signal to help you avoid further injury.
Illnesses are also a common cause of pain. Certain conditions, such as arthritis or fibromyalgia, can lead to chronic pain that persists for extended periods of time. In these cases, the pain isn’t a temporary response to an injury but a symptom of an underlying condition. Managing pain caused by illnesses requires a comprehensive pain management approach that addresses both the physical and emotional components of the condition.
Pain can also be caused by inflammation. Whenever your body detects an injury or infection, it releases chemicals that cause inflammation as a way to facilitate the healing process. And while inflammation is necessary for your body to begin to heal, it can also cause pain and discomfort. For example, conditions such as tendonitis often result in localized inflammation, causing pain in a specific area of your body. Pain management protocols for this type of pain focuses on reducing the inflammation itself.
Finally, did you know that stress is another common cause of pain? In fact, research has shown that stress and anxiety can lower your threshold for pain. In these cases,addressing the psychological component of pain is crucial, and pain management often includes relaxation techniques, therapy, or certain stress management strategies.
By understanding both the physiology of pain and what causes pain, you can begin to empower yourself to make informed decisions about your own pain management. You can begin to have more meaningful conversations with your pain management doctors and actively participate in your personalized treatment plan. But before we begin to unfold the world of pain management, let’s quickly take a look at the two major types of pain: acute vs chronic.
Acute Pain vs. Chronic Pain
Pain is categorized into two main types: acute pain and chronic pain. Acute pain is a type of pain that is short-lived and often serves as a way to protect your body from danger or further damage. It’s often associated with tissue damage resulting from an injury or even surgery.
Conversely, chronic pain lasts for longer periods, often extending beyond the expected healing time of an injury. It can be caused by conditions such as arthritis, nerve damage, or even psychological factors.
Within the two major types of pain are a few specific manifestations. The first is nociceptive pain, which occurs due to tissue damage resulting from an injury, inflammation, or an underlying condition. The second is neuropathic pain, which occurs due to damage to your nerves. It’s often described as shooting or burning. Finally, the third is psychogenic pain, which is tied to psychological or emotional factors and feels like a deep, aching pain. It’s typically influenced by stress, anxiety, depression, or another mental health-related condition.
By understanding the characteristics of these different types of pain, you can work with your pain management doctors to create tailored treatment plans to address your specific needs. Now, let’s take a closer look at pain management to better understand the options available to you.
What Is Pain Management?
So, exactly what is pain management? It refers to the multidisciplinary approach for alleviating, reducing, or controling pain. Pain management involves the use of different techniques, interventions, and therapies tailored to each person’s specific needs. Ultimately, the goal of pain management is to enhance your body’s ability to function optimally, improve your quality of life, and minimize the impact of pain on your daily activities.
Anyone who experiences chronic pain that affects their daily life can benefit from pain management. From athletes with sports-related injuries to those living with chronic conditions, pain management strategies can help restore a sense of normalcy and help to alleviate unnecessary suffering.
Types of Pain Management
There are several different approaches to pain management, and each is best suited for different types of pain and circumstances. Here’s a closer look at the different types of pain management, from over-the-counter to more advanced pain management.
Medication for Pain Management
Pharmaceutical interventions are common in the world of pain management — but that doesn’t mean they’re the best or even necessary for most types of pain.
Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, and anticonvulsants are known to provide relief by targeting certain pain pathways, but they come with a variety of harmful side effects and risks. In fact, you may be surprised to learn that conventional pain medications are designed to manage the decline of the joint tissues and nerves that cause pain. The truth of the matter is that doctors often prescribe anti-inflammatories or steroids with the hope of simply buying you some time before you have to undergo an inevitable procedure or surgery.
For example, let’s assume you have arthritis in your knee. Conventionally, doctors will prescribe a steroid as the first approach for relieving pain associated with an arthritic knee. But by wiping out the inflammation, which is the source of the pain but also your body’s attempt to heal your knee, the steroid damages your tissue even further, especially when it’s used over a longer period of time. So, while you’re pain-free for a short amount of time, this medication causes more wear and tear on the tissues in your knee, causing them to wear down faster and ultimately accelerate your surgery date.
Likewise, anti-inflammatory drugs and muscle relaxers target the inflammation, which can help to relieve your pain for a bit, but these medications come with a variety of side effects, including the tendency to bog down your liver (which has the important job of supporting your body’s ability to fight and eliminate toxins).
By taking these medications, you may experience some time feeling pain-free, but you’re now faced with the dilemma of having dysfunction in your liver and even your gut, as anti-inflammatories are known to actually eat holes and/or cause ulcers in your gut.
The result? Yet another acceleration to your surgery date. And that inevitable surgery isn’t even a guarantee of finally being pain-free. In fact, surgery failure rates are high, and they’re even known to cause even more long-term complications? It’s actually very common to see that once you fuse one joint together in surgery, the joints below and above the fusion become damaged due to further wear and tear. Plus there’s the increased likelihood of experiencing neuropathy pain, scar tissue, and more after surgery.
As you can see, it becomes a cycle of inevitable long-lasting pain and concerns. As a result, here at The Dearing Clinic in Nashville, we recommend pursuing other forms of pain management first. Keep reading to learn about other options available to you.
Drug-Free Approaches to Pain Relief
Drug-free pain management approaches offer alternative techniques to help manage or even eliminate pain without the harmful side effects of their pharmaceutical counterparts. These methods include physical therapies (such as contrast therapy, peptide therapy, IV therapy, chiropractic care, and structural rehabilitation), cognitive-behavioral therapies, relaxation techniques, and more. Adopting these approaches can aid in relieving pain and promote overall well-being. Here are a few drug-free pain management therapies to consider.
Alternative Therapies for Pain Management
In recent years, alternative therapies have gained popularity as standalone or complementary pain management strategies with up to 90 percent of patients dealing with musculoskeletal pain reporting relief from alternative therapies. As such, natural pain management techniques including herbal medicine, aromatherapy, yoga, and meditation have shown promising results in reducing pain symptoms.
Additionally, physical therapies have shown amazing benefits for pain management. For example, contrast (or hot and cold) therapy benefits your entire body and autonomic nervous system while naturally helping to fight inflammation and promote the healing process, making it an excellent therapeutic option if you’re wanting to manage pain naturally.
Meanwhile, other physical therapies such as structural rehabilitation, trigger point injections, chiropractic care, and IV therapy are known to improve energy levels by encouraging your tissues to heal locally while also encouraging your body’s ability to heal systematically by increasing your metabolism. And by boosting your metabolism, this has a beneficial effect on every cell in your body — and all without the unwanted side effects that come with pharmaceutical medications.
This list of alternative therapies is by no means comprehensive, so make sure to speak with a qualified pain management specialist to learn more about the options available to you. You can also contact The Dearing Clinic to speak with one of our team members to learn more about our pain management offerings.
Psychological Strategies for Pain Management
Other alternative therapies include psychological strategies, and that’s because managing pain is about more than just physical interventions; it also requires addressing the emotional and psychological aspects. Psychological strategies, such as cognitive-behavioral therapy, mindfulness-based stress reduction, and relaxation exercises, can help you develop coping mechanisms, reduce anxiety, and enhance your resilience for pain.
If you think you may benefit from incorporating psychological strategies into your pain management plan, speak with your physician about your personal health situation to determine if this is the right adjunct therapy for you.
Lifestyle Changes that Support Pain Management
Adopting certain lifestyle changes can significantly aid in your pain management plan. Specifically, consuming an anti-inflammatory diet, incorporating regular exercise (including strength training), and prioritizing both quality sleep and stress reduction can help to reduce your pain levels. Additionally, consider engaging in activities that you enjoy, such as picking up certain hobbies or creative pursuits, to help improve overall your well-being.
What Do Natural Pain Management Doctors Do?
Now that you know more about how pain management works and the options available to you, let’s take a look at what natural pain management doctors do to help you find relief.
Natural pain management doctors specialize in diagnosing and treating various pain-related conditions. Using a wide range of techniques including physical examinations, diagnostic tests, interventional pain management procedures, and patient education, natural pain management doctors play a crucial role in coordinating a patient’s overall pain management care plan. They prioritize the use of drug-free approaches and tailor your treatment plan according to your personal health history, the origin of your pain, and your personal health goals. Pain management doctors often work in either a pain management clinic or in a hospital office setting.
When seeking care from a natural pain management doctor or pain specialist, remember that this is a deeply personal journey for you that requires patience, resilience, and a willingness to explore different strategies. By understanding what causes pain, identifying the pain’s sources, and utilizing the appropriate interventions and healthcare practitioners, you can take control of your pain and begin your journey towards improved well-being.
Key Takeaways
- Whenever you experience pain, it’s only natural to want immediate relief. But there are many different comprehensive pain management options available for your consideration.
- It’s important to work with a pain management doctor or specialist to determine the cause of your pain so that you can determine the best approach.
- Unfortunately, treating pain symptoms with medication will only buy you extra time, while some pain meds are actually known to worsen the problem and cause even more issues — and possibly even a sooner surgery date!
- To get to the root cause of your pain and find lasting relief, consider reaching out to a pain management doctor at a local pain clinic who specializes in natural pain management and takes a truly comprehensive approach.
- Effective natural pain management options include contrast therapy, peptide therapy, IV therapy, chiropractic care, structural rehabilitation, cognitive-behavioral therapies, relaxation techniques, and more.
Ready to feel like you again?
* Your next step toward feeling better starts today. At The Dearing Clinic we make it simple to get started with care that truly fits your life. Book your visit now and let’s design a plan that restores your energy, relieves your pain, and helps you enjoy more of what matters most.